Circulating HPV DNA as a Marker for Early Detection of Relapse in Patients with Cervical Cancer
Abstract
Purpose:
Almost all cervical cancers are caused by human papillomavirus (HPV) and patients with advanced stage are at high risk for relapse. Circulating HPV DNA (HPV ctDNA) may serve as a residual tumor marker at the end of chemoradiation or to predict relapse during the follow-up period.
Experimental Design:
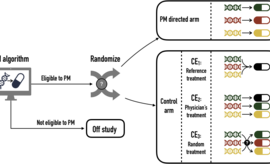
We analyzed serum samples from 94 HPV16- or HPV18-related CCs from the BioRAIDs prospective cohort. Samples were collected before and after treatment and during an 18-month follow-up period. Using digital droplet PCR (ddPCR), we assessed the relevance of circulating HPV E7 gene as a marker for residual disease compared to HPV integration site and PIK3CA mutations. Finally, the prognostic impact of circulating HPV E7 gene was assessed with its prediction value of relapse.
Results:
HPV E7 gene was the most sensitive tumor marker, superior to both HPV integration sites and PIK3CA mutations in serum. Circulating HPV DNA (HPV ctDNA) was detected in 63% (59/94) of patients, before treatment. HPV ctDNA detection in serum sample was associated with high FIGO stage (P = 0.02) and para-aortic lymph node involvement (P = 0.01). The level of HPV ctDNA was positively correlated with HPV copy number in the tumor (R = 0.39, P < 0.001). Complete clearance of HPV ctDNA by the end of treatment was significantly associated with a longer PFS (P < 0.0001). Patients with persistent HPV ctDNA in serum relapsed with a median time of 10 months (range, 2–15) from HPV ctDNA detection.
Conclusions:
HPV ctDNA detection is a useful marker to predict relapse in cervical cancer.
See related commentary by Wentzensen and Clarke, p. 5733